
Ipswich Hospital
Ipswich Hospital NHS Trust provides secondary (specialist) or acute healthcare to a core catchment population of approximately 356,000 people living in Ipswich and East Suffolk. It is a busy district general hospital with 631 beds in general acute, maternity, paediatric and neonatal services
In June 2008, The Garrett Anderson Centre was opened, which provides a new Emergency Department, a 22 bed Intensive Care facility, 40 elective surgery beds and 4 operating theatres with associated day case surgical unit. The Urgent Care Centre was rated as Outstanding by the CQC Inspection in April 2015.
| Address: | Heath Road Ipswich Suffolk, England |
| Phone: | 01473 712233 |
| Founded: | 1810 |
| Number of Beds: | 800 |
| Educational Supervisor: | Mr Servant |
| Rota Co-Ordinator: | Jan King - Jan.King@ipswichhospital.nhs.uk |
| Website: | http://www.ipswichhospital.nhs.uk |
| Human Resources: | Debbie Allum |
| Trauma Co-Ordinator | Matron - Jan Wright bleep 650 |
Welcome to the Trauma & Orthopaedic Department in Ipswich. This page will provide you with useful information specific to working as a SpR here.
Rota
Consultant rota
In Ipswich the T&O Consultant on-call system is a daily on-call system:
- 12 Consultants do a fixed weekday (Mon-Thu) 1:3 rota and work 1:12 weekends (Fri-Sun), although some Consultants split the weekend
- The on-call day runs from 08:00 to 08:00
Emergency admissions are admitted under the care of the Consultant on-call at the time the referral is accepted.
Each on-call day usually runs as follows:
- 08:00 Trauma Meeting (chaired by the Consultant on-call the previous day)
- 08:30 Fracture Clinic, including all new outpatients referred within the previous 24 hours (not Sat and Sun – Fri and Sat referrals are seen by the weekend Consultant on Mon)
- PM Administration: the Consultant may usually be found in his office
Following day:
- 08:00 Trauma Meeting
- Trauma Ward Round
- Trauma List in Lavender Theatre (in the South Theatres complex): 08:30 to 17:00 Monday to Friday, 08:30 to 13:00 on Saturday and Sunday
There is a separate spinal Consultant on-call rota.
The Consultants do not carry bleeps but may be contacted on their mobile phones or via switchboard.
SpR rota
During the weekday the on-call SpR may be scheduled to be in theatre, in which case a colleague must hold the 300 bleep as the bleep holder should always be available to answer the bleep promptly.
The on-call SpR is non-resident after 22:00 but is still part of the Trauma Team and is required to be able to attend the ED within 15 minutes of being contacted (even when non-resident).
The on-call SpR has the day off following being oncall.
Junior doctor rota
The on-call junior doctor (FY2/CT level) covers T&O during the day, and T&O / General Surgery overnight.
Annual Leave
You must complete a leave request form for all leave. This will need to be signed by your team Consultant and the rota co-ordinator (Mr Al-Nammari). You must give a minimum of 6 weeks’ notice (ideally 8 weeks) to allow time for clinics and /or operating lists to be adjusted accordingly.
No more than 3 SpRs will be allowed leave at any one time, except under exceptional circumstances. You are encouraged to book blocks of leave rather than single days.
Study Leave
A study leave form (pink form) must also be completed for all study leave.
Consultants
Weekly timetables and consultant pairings can be found here. Your exact commitments should be discussed with your Clinical Supervisor (team Consultant). Wherever possible, you should attend the Trauma Meeting each weekday morning.
Consultant allocations and cross-cover
During periods of SpR leave certain duties may need covering (e.g. new patient Fracture Clinics, responsibility for the management of a Consultant’s in-patients). To help in determining who should provide the cover, the Consultants have been grouped into teams and, wherever possible, the SpRs in a team should cross-cover each other (see Appendix 2).
Clinics
The hospital has an electronic patient record system (evolve), which is used to store some, but not all, patient records.
In general, all new patient Fracture Clinics should be covered by a SpR.
Theatres
You will attend your consultants elective and trauma operating list. Should you work for two consultants, you will always go to the trauma list over the elective list.
Teaching
Mr Servant runs a weekly teaching programme at 5.30pm on Tuesdays. The teaching will compromise a mixture of journal clubs, lectures, evidence-based debates on controversial topics, case discussions and viva practice.
All SpRs (including the on-call SpR) are encouraged to attend the regional teaching on Thursday afternoons.
Audit & Research
Mr Al-Nammari is the Consultant responsible for Audit. Mr Roberts is the Consultant responsible for Research.
Junior Trainee Mentoring
Chris Lawrence, one of the 2013-14 SpRs, started a mentoring programme that allocated a named Registrar mentor for each junior doctor. Further details are given in a separate document: ‘Mentor Handout Aug 15’. This has proved to be very useful and the programme continues.
Educational Supervisors
I am your Speciality Tutor. 3 other Consultants and I will share the role of Educational Supervisor – please refer to the separate list to find out your allocated Educational Supervisor. Your Educational Supervisor will not be one of your Clinical Supervisors.
You should ensure that I (as your Speciality Tutor), your Educational Supervisor and your Clinical Supervisor all have access to your ISCP record.
- Formal meetings with your Clinical Supervisor(s): you should arrange initial, mid-point, and end-of-placement meetings: first month, third / fourth month and sixth month of each 6-month placement.
- Formal meetings with your Educational Supervisor: please arrange a meeting at the beginning of each placement (to complete a learning agreement), and at the end of each placement, i.e. August, end-January or early February and June (before your ARCP in July).
- You should achieve or be on track to achieve certain targets (or waypoints) to improve your chance of a successful outcome at your next ARCP. Further details are on the JCST website: www.jcst.org/quality-assurance/certification-guidelines
- You should also keep your ISCP portfolio up-to-date, including uploading a current CV immediately prior to your ARCP.
I am always happy to address any questions or discuss any problems, issues or suggestions for improving the training in Ipswich.
Chris Servant
August 2015
Ipswich Spinal Unit
The Ipswich spinal unit consists of 5 consultant spinal orthopaedic surgeons, 2 rotational registrars and 2 fellows. The unit is supported by 4 surgical nurse practitioners. The unit offers a full elective and trauma spinal service and has access to 24/7 MRI facilities.
Surgical Emergency Service
The Ipswich Hospital offers a comprehensive 24/7 on call spinal service.
The spinal surgical unit offers an emergency service to cover all aspects of spinal surgery including:
- Cauda Equina
- Spinal Fractures
- Spinal Infections
- Metastatic spinal disease including MSCC.
The spinal unit also offers access to an acute spinal clinic that is run by the on-call spinal surgeon weekly. This clinic is accessed via the spinal secretaries.
Referral Guidelines
All GP referrals & A/E referrals should be made to the orthopaedic on call service.
All ward referrals from within Ipswich Hospital should be made via the orthopaedic on-call registrar. The registrar is contactable via The Ipswich Hospital Switchboard (Bleep 300).
The cases can then be discussed after assessment with the spinal on-call team.
It is expected that the orthopaedic registrar on-call overnight will contact the spinal consultant at 0730 each morning to discuss any cases referred &/or admitted overnight, that have not already been discussed.
If an MRI scan is required out of hours. The on-call registrar will assess the patient and discuss directly with the on-call spinal consultant.
Tertiary Referrals (West Suffolk Hospital, Colchester Hospital, Mid-Essex Hospital)
All tertiary referrals in normal working hours (0830 – 1700) are taken by the spinal service on 07467 069656. If the orthopaedic registrar is contacted by another hospital, they should take the details of the referral and forward to the spinal on-call team.
1700 – 0830 Monday to Friday, weekends & bank holiday’s – registrar to registrar referral via switchboard at Ipswich Hospital.
No patient should be transferred to Ipswich Hospital without the agreement of the spinal
consultant.
All tertiary referrals should also have a Acute Spinal Referral Form completed along with an ASIA Chart.
Accommodation information - http://www.ipswichmanagement.co.uk

The West Suffolk Hospital is a vibrant, friendly and accessible hospital set in a 19-hectare parkland site on the edge of Bury St Edmunds. It has around 430 beds open at any one time and serves a population of around 275,000 within area of approximately 600 square miles. It is easily accessible by road via the A14 and is approximately 30-40 minutes from Cambridge. Bury St Edmunds in Suffolk is a unique and dazzling historic gem. An important market town with a richly fascinating heritage, the striking combination of medieval architecture, elegant Georgian squares and glorious Cathedral and Abbey gardens provide a distinctive visual charm.
Trauma and Orthopaedics Information
We are a cohesive and proactive group of 12 consultants and one associate specialist covering the usual sub-specialities. There are 7 Lower limb arthroplasty surgeons, 3 foot and ankle and 3 upper limb. Spines are covered by Ipswich.
Whilst at the West Suffolk there is lots of opportunity to progress both clinically and academically. As a group we will support and prepare you for the FRCS and your life in orthopaedics.
There are 9 registrars, 5 of whom are regional trainees. The others are on rotation from Sri Lanka, Belgium and Egypt. Registrars tend to be year 1-4 and rotate through at least 2 consultants, one every 6 months. Some Consultants are linked so the registrar works for 2 at the same time.
On calls are covered by one of 10 consultants who work from Monday 8am –Thursday 5pm or Thursday 5pm – Monday 8am. When on call the consultant has no elective duties. The registrars work a 24 hours on-call with the next day off rota and an on-call room is provided. There are foundation doctors both on the wards and covering the on-calls.
Working with us there is also a Consultant orthogeriatrician, 6 nurse practitioners and 2 trauma nurse practitioners. They all play a vital role in the running of the department and are highly qualified and regarded.
The timetable for the whole department is kept on medirota and is available on any computer or on your phone as an app. You will be given access to this once you arrive but guest access can be given, if required, once you know you are allocated to rotate here. Registrars cross cover clinics and theatre for their colleagues. The usual 6 weeks’ notice is required for leave unless in exceptional circumstances.
Your educational supervisor here is Miss Lora Young ( lora.young@wsh.nhs.uk)
Rota/ medirota co-ordinator is Bev London (bev.london@wsh.nhs.uk)
Human resources are available on 01284 713528
West Suffolk Hospital Orthopaedic Department

- 430 beds
- Population of around 275,000
- The West Suffolk is a district general hospital situated in Bury St Edmunds.
We are:
- 13 consultants and one associate specialist
- 8 Lower limb arthroplasty
- 3 foot and ankle
- 3 upper limb surgeons.
- Spines are covered by Ipswich.
Whilst at the West Suffolk Hospital there are lots of opportunity to progress both clinically and academically. You will be supported and given a mix of opportunities in theatres and clinics. As a group, we will support and prepare you for the FRCS and your life in orthopaedics.
Key Contacts
Address: Hardwick lane, Bury St Edmunds, IP33 2QZ. Tel: 01284 713000
Educational Supervisor: Miss Lora Young
Rota Co-ordinator: is Mr Konrad Wronka
Rota secretaries- Sheenagh Bugg sheenagh.bugg@wsh.nhs.uk//Bev London Bev.London@wsh.nhs.uk

Consultants and pairings
Rota
- 9 registrars
- 5 regional trainees
- 3 trainees on Fellowship (Belgium/ Sri Lanka)
2x consultant pairings as clinical supervisors per 6month block.
On calls
Consultants on call blocks Monday 8am-Tursday 5pm and Thursday 5pm- Monday 8am. During on call, elective operations for that consultant surgeon are cancelled but clinics will continue. Registrars work 24 hours on-call with on call accommodation provided and compensatory rest day the following day. There will be cross covering of clinics to account for leave.
The team
- Foundation/ GP trainees on 4/12 rotations wards & on call
- consultant orthogeriatrician
- 2 trauma nurse practioners
- 1 advance care practioner
- surgical nurse practioners
- fracture clinic physiotherapists
- Plaster team
- Children nurses
- Fracture clinic nurses. … And many, many more
IT
Rota on Medirota (app) – records whole department rota.
Bleeps through Medicbleep (app)
Electronic patient notes (E-care)
Nurse Specialists
7 nurse specialists help in both clinics and theatres. They will be support in clinic and theatres.
- Donna Taylor – Upper limb
- Sue Lafflin – Arthroplasty (Mr Schenk and Mr Nicolai)
- Sara Davey – Hip (Mr Parsons, Mr Shakokani and Mr Al-Hadithi)
- Sarah Reader – Hip and Knee (Mr Dunn and Mr Shakokani)
- Gemma Salt – Foot and ankle (Mr Vaughn) Hip (Mr Atrey)
- David Higgins – Foot and ankle
Leave
Annual leave can generally be taken when suits the individual. It is however important to ensure not too many SPR’s are off at any one time. (Usually 2 but exceptions can be made if it is possible to cover all clinical work).
Leave should be booked through contacting Bev London or Sheenagh Bugg. It is recommended you email both and try to catch them in person (Ortho Offices). As the Medirota is planned 6 weeks in advance it is necessary to give 6weeks and ensure commitments are covered.
Clinic
During COVID-19 Clinics are currently arranged as Super clinics per subspeciality of the same day each week. These will be a mix of elective planned follow up triage clinics and fracture clinics.
The previous system was based upon 2 clinics per session (morning/afternoon) to include a mix of elective and orthopaedic patients specifically for that consultant. These clinics will always be run by 2- either consultant and registrar or two registrars depending on rota commitments and leave. You will need to cross cover clinics to accommodate leave, post night oncall etc, which will be scheduled on Medirota.
Virtual Fracture Clinic
This is a patient free clinic that runs every weekday starting at 7.30 and will consist of named consultant, secretary and fracture clinic team member. Both A&E and GPs refer to this clinic for patient referrals.
On call at Night
The on call’s are a 24hr non-resident shift. The registrar should remain on site till 10pm and then transfer the bleep to switchboard on medic rota.
As the on calls are non-resident, an on-call room is available off site as you will be expected to available to come into hospital if needed within 20 minutes. The key to this room is on a lanyard and should be left in the registrar office.
There is one SHO overnight covering orthopaedics, general surgery and urology. The following day is given off as a rest day. The rota is a rolling rota and therefore is a fair as possible in terms of cover for weekends and bank holidays.
Prior to 10pm, the registrar is the first on call. After 10pm all GP and A&E referrals will go to the night surgical SHO. Any new patients admitted overnight will need to be seen by the night registrar prior to the trauma meeting.
Swaps
As there will be rest days off during the week following on call some regular commitments may be missed from time to time however due to the rolling nature of the rota the same things should not be missed all the time. You are welcome to swap these on calls to balance your commitments and to ensure the rota is updated please flag up any swaps to both Bev and Sheenagh and these can be accommodated on the rota. Please email all swaps including the swapping registrar to Sheenagh and Bev. If you wish to take leave when you are, meant to be on call it is your responsibility to swap out of these on call shifts. If you need to take your leave for longer periods for example honey moons, long travel please do give as much notice as your case and discuss this request with rota team.
Trauma Meeting
Trauma meetings take place at 8am every morning in the discussion room on the F3/F4 corridor. These should be attended by everyone whenever possible.
All patients seen during the on call, awaiting surgery, requiring results follow up or immediately post op or have any concerns that need to be shared with the juniors/ consultant team are included. These patients are added to this Trauma list via e-Care.
Trauma Booking
The SpR should have marked and consented the patient. They will need to book the patient for theatre by E-Care as a ‘TRA’ trauma case or ‘EMER’ emergency case. These should also be written down on a red clipboard for the relevant day, held by theatre teams in the theatre coffee room.
Each patient needs A VTE assessment and appropriate VTE prescribed along with a EPARS resuscitation decision and discussion. Please also call the family and include them in DNAR discussions.
Booking Paperwork
- Yellow consent form
- Pink WHO checklist form
Both must be done along with EPARS and VTE for patient to be transferred to theatre for surgery.
Theatres
Theatre 3 – Emergency theatre shared with all surgical specialties and runs 24/7.
Theatre 7- Elective orthopaedics – Mon-Fri 9am-5.30pm
Theatre 8 – Trauma theatre- Every weekday 1.30-5.30pm; Weekends varied schedule.
Theatre 9- Elective Orthopaedics Mon-Fri 9am-5.30pm
Day surgery Unit (DSU) – elective/ planned trauma facility; varied sessions.
Wards
F1 ‘Rainbow ward’ – Paediatrics
F3- trauma and Spine
F4- Elective (need MRSA -ve swab)
F6/7- general surgical/ surgical outliers wards.
Comments
WSH is a wonderful place for training and working. You have won the lottery with your placement! Enjoy your time here.
Accommodation
The accommodation office is responsible for all aspects of the day to day running of the staff accommodation blocks and the welfare of the residents.
Contact details
Accommodation Officer: Lizzie Johnson
Tel no. 01284 713491
Fax no. 01284 713875
E-mail: accommodation@wsh.nhs.uk
Opening Times
Monday - Thursday 8am - 4pm
Friday: 8am - 3pm

Norfolk and Norwich University Hospitals NHS Foundation Trust (NNUH) is one of the largest NHS trusts in the United Kingdom and provides first-class acute and specialist services. The job of the hospital is to provide the best possible care for a tertiary catchment area of up to 1 million people. It is easily accessible by both rail and motorway (through the A11 highway) and it is approximately two hours’ commute from London. The city itself has a large range of shopping facilities and is close to the broads (an area of outstanding natural beauty).

NNUH Accommodation is situated within the grounds of the Norfolk and Norwich University Hospital. 144 ensuite single rooms with limited twin rooms also available for couples. Accommodation available for nightly, weekly or monthly stays.
The Accommodation Office is closed outside office hours. In case of emergency contact the main Hospital Switchboard 01603 286286 and you will be put through to our out of hours service.
Sarah Smith, Accommodation Manager, Accommodation Office, Norfolk and Norwich University Hospital, Colney Lane, Norwich, Norfolk, NR4 7UP
OPENING TIMES
Monday 07:30 – 18:00
Tuesday 07:30 – 18:00
Wednesday 07:30 – 18:00
Thursday 07:30 – 18:00
Friday 07:30 – 15:30
Saturday closed
Sunday closed

|
Address: |
Turner Rd, Colchester CO4 5JL |
|
Phone: |
01206 747474 |
|
Founded: |
1984 |
|
Number of Beds: |
562 |
|
Educational Supervisor: |
Mr Loeffler |
|
Rota Co-Ordinator: |
Most senior SpR |
|
Website: |
|
|
Human Resources |
Jade.cooper@colchesterhospital.nhs.uk |
|
Trauma Co-Ordinator |
Welcome to Colchester Hospital University NHS Foundation Trust (CHUFT), situated in Britain’s oldest recorded town, Colchester. It is easily accessible by both rail and motorway (through the A12 highway) and it is approximately an hours’ commute from London. Alternatively there is a train that originates from Liverpool Street, London). The trust serves a district population of approximately 334,000 with a high proportion of elderly people, and as a trainee you will be exposed to a wide variety of clinical conditions and pathologies. The town itself has an active town centre and many amenities are nearby such as supermarkets and gyms.
A busy orthopaedic department with 12 consultants some are paired together:
- Lynn Barre- foot and ankle
- Georgina wright- foot and ankle
- D’Jon Lopez - hip
- Shiv Shanker – Paediatrics
- Williams – Foot and Ankle
- Sloper – Lower limb arthroplasty
- Wardle – lower limb arthroplasty
- Stanton – upper Limb
- Loeffler – Lower limb arthorplasty and soft tissue knee
- Alam- Knee soft tissue + Arthroplasty
- Suresh – Spines and lower limb mix & Blackman – Spine
- Hynes – Upper limb
Induction
This is done by Mr Sloper usually. He will give you a booklet on arrival. Bleep system is 7575 then bleep number then message. There is no SpR office! Wards are Great Tey for elective, Aldham for Male Trauma and Fordham for Female trauma. There is lots of e-learning! They send this to you to
complete before you go and say they will pay you for it but the computer system is not very good at working out what you have and haven’t done so trying to get that pay is difficult. Notes are all paper based. Bloods on ICE, discharges also. There is a separate VTE computer programme and
another one for theatre lists. Bighand for all electronic dictations.
Rota
1 in 9 on calls, currently there are two registrars from the East of England and three from the East London rotations, however these posts are in the process of being repatriated to the East of England. The department all has three staff grades.
The most senior registrar is the rota co-ordinator (for the registrar and SHO rota).
Registrars are on call for 24 hours, being non-resident after 5pm in the week. At the weekend on call from Saturday 8am to Monday 8am (again non-resident after 5pm each day).
A trauma list runs 08:00 – 17:30hrs including Saturday and Sunday. The SHO is 1st on call at all times. Unless you are unsafe to work you do not receive a compensatory rest day following on calls.
Theatres
You operate with the consultant and supervision depends on ability. Trauma is supervised but if the consultant is away you may be given cases to do on the list if you and the consultants are happy. If the consultant is away you cover the trauma list session.
Clinics
You have your own clinic running alongside the consultant clinic. This will continue to run if the consultant is away unless they deem you to need close supervision. No cross cover – 6 weeks notice for leave and then the clinic is cancelled.
Teaching
Lunch time meetings on Thursdays are aimed mainly at SHO level as the East of England registrars have regional teaching then.
Daily trauma meetings offer teaching dependant on the case mix and consultant. Questions are welcome.
Trainee Comments
Colchester is a great place for getting some independent experience and operating on your won (depending on your skill) The bosses are all approachable and helpful. The SHO rota is patchy and there are several locums which can make the on calls a bit annoying. The CQC visit frequently and as a result changes keep getting made.

Luton and Dunstable University Hospital
Lewsey Rd
Luton
LU4 0DZ.
Telephone - 01582 491166
Founded : 1937 Number of Beds: 500
Educational supervisor: Mr Yega Kalairajah
Rota coordinator: Helen Blunt ( ec to Mr Burtt/Mr Manjure)
Orthopaedic Department
The Orthopaedic Department in Luton and Dunstable Hospital is a busy trauma and elective unit in the region providing care for trauma patients and elective orthopaedic cases both in general as well as sub-specialised areas e.g. Upper Limb, Hand, Foot and Ankle, Spine, and Lower limb. Each year the Orthopaedic Department performs over 5,000 orthopaedic surgical procedures for patients from Bedfordshire, Hertfordshire and beyond. There are 11 Consultants and 2 designated Trauma Surgeons. Mr Yega Kalairajah is the consultant lead for training.
Lower limb firms provide high volume arthroplasty exposure including computer navigation technology for knee arthroplasty
Three orthopaedic theatres run every day - 2 elective and 1 trauma theatres. There is a half day dedicated trauma list on Saturday and Sunday which is run by trauma surgeons.
There are excellent opportunities for trainees to acquire surgical skills in routine orthopaedic trauma due to high numbers and availability of Consultants or experienced Senior Surgeons to supervise trainees.
Rota:
A shift system is in place with 12 hour resident on-call shifts. Trainees are not allocated to night shifts to avoid missing opportunities of training due to compensatory days off.
Theatres and Clinics
Average week for trainees includes:
1 elective and 1 fracture clinic,
1 full day elective theatre with respective consultant,
3 half day trauma theatre sessions at least,
1 half day research/CME session.
Protected Thursday afternoon for SPR teaching.
Teaching and training
Teaching sessions include a trauma meeting every morning, Wednesday lunch time Journal club session and a Friday metalwork meeting.
Every 2 months there is an evening workshop organised with the industry representatives to provide saw bone sessions for new registrars and familiarise with the systems used the hospital.
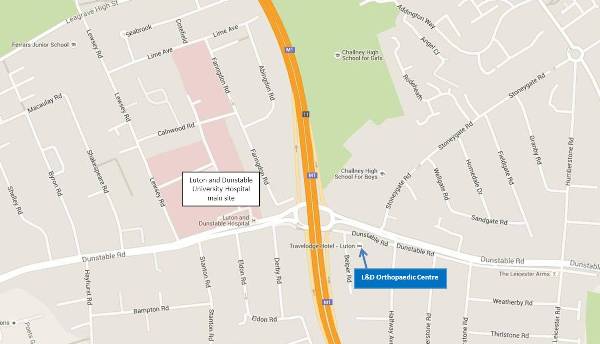
Map
Induction information:
Registrar induction information is sent to all new registrars. There are some compulsory on line induction modules that need to be completed in order to be allowed access to the different applications required to access paperless patient notes and scans as all systems are computerised.
List of useful contacts (i.e. HR / rota co-ordinator / educational supervisor contact details):
Hospital Switchboard: 01582 491166
Helen Blunt. Orthopaedic Rota Coordinator: Helen.blunt@ldh.nhs.uk Ext 8203
Louise French. HR Department and Surgical Rota Coordinator: Louise.French@ldh.nhs.uk Ext 8472
Helena West. HR Department: Helena.West@ldh.nhs.uk Ext 8257
Sister Anne Barker: Trauma Coordinator Bleep: 268
Educational Supervisor: Yegappan.Kalairajah@ldh.nhs.uk Sec Rita Ext 7068
Any further information you feel is relevant, e.g. highlighting department strengths:
“Extremely busy Department but as a reward there are plenty of operating and training opportunities available. Friendly and supportive staff. Designated Orthogeriatric team who help deliver multidisciplinary approach to fracture neck of femur care. “

Addenbrooke’s Hospital
| Address: | Hills Road, Cambridge, CB2 0QQ |
| Phone: | 01223 245151 |
| Founded: | 1766 |
| Number of Beds: | 1,180 |
| Educational Supervisor: | Mr Kang |
| Rota Co-Ordinator: | Senior SPR - currently Andrea Bardos |
| Website: | http://www.cuh.org.uk |
| Human Resources: | |
| Trauma Co-Ordinator: | Bleep 156-189 |
Addenbrooke's hospital, Cambridge, is one of the largest and well known hospitals in the UK.
The trust provides emergency surgical and medical care for local people and is also a regional centre of excellence for specialist services such as organ transplantation, neuro sciences, paediatrics and genetics.
Based on the same site the Rosie is a womens hospital and the regional centre of excellence for maternity care.
Addenbrooke's is a government designated biomedical research centre and is one of only five academic health science centres in the uk.
Rota/ on call commitments
Full shift pattern with resident on call night shifts.
In any 12 month period, you do 3 x 1 month blocks of on call with a mixture of days on call and nights on call. You are free from all elective work during this time.
On calls are shared between SpRs and middle grades with middle grades doing more on call and covering elective SpR work when they are away.
SpRs are first on call day or night. SHOs are F2s to CT2s.
Epic – Addenbrooke’s is paperless (except for consent forms). There are good things about Epic but it is hard work to navigate and to get the most out of it.
Teams
The consultant teams are organised into pods; the purpose of this is to reduce the need to cross cover between specialties during leave etc and allow continuity of care for patients. Registrars are allocated formally to one or two consultants but will usually work with all consultants in their pod at various times.
Pod A
Mr Hull* / Mr Vince – P&A / Arthroplasty
Mr Rawal* – P&A
Mr Carrothers* – P&A
Mr Khanduja – Hips
Pod B
Mr Chou* / Mr Gooding – P&A / Arthroplasty
Mr Keene – Hips
Mr Owen – Hips
Pod C
Mr Krkovic* – Lower limb recon
Mr Edwards / Mr Melton – Knees
Mr McDonnell / Mr Khan – Knees
Pod D
Miss Ashby / Mr Rehm – Paeds
Miss Stohr – Paeds
Mr Latimer / Spine – Paeds and spines
Mr Robinson – Foot and ankle (just has a fellow)
Pod E
Mr Johnston / Mr Hopkinson-Woolley – Hands
Mr Kang / Mr Johnston – Shoulders / Hands
Mr Van Rensburg* / Mr Tytherleigh-Strong – Shoulders
*major trauma consultants
Theatres
Most operating is done at Addenbrookes. There are two trauma theatres: Th16 for MTC trauma and Th17 for DGH trauma.
Some consultants do day case elective lists at The Princess of Wales Hospital, Ely.
Clinics
Clinics are mostly clinic 1 (hands in clinic 5), ground floor in the main outpatients’ department. Requests, documentation, follow up is all done on Epic.
Teaching and training
The trauma meeting involves teaching depending on which consultant has been on call. The Friday morning OTU meeting does involve teaching.
Handover
Main trauma meeting:
- T&O seminar room on C8
- between 7 and 8am depending on the consultant
OTU handover meeting:
- level 2 neuro library, next to NCCU/ J2 seminar room on Fridays
- 7:30am
Contacts
Rota coordinator: Andrea Bardos
Chief Educational Supervisor: currently Mr Kang
Pelvic & Complex Trauma Referrals
Referring hospitals should complete all referral documentation and ensure images have been sent via TRAD/PACS system.
Referral documentation available on: www.cambridgepelvicsurgery.co.uk
All Pelvic & Acetabular referrals: add-tr.cambridgepelvis@nhs.net
Major Trauma Patients requiring Emergency Surgery
For patients that require emergency trauma surgery Monday to Friday between the hours of 08.00 to 19.00. Please contact Theatre 16 (58036) and discuss with OTU Consultant on call. These do not require discussion with the on call consultant of the day.
Repatriations
For patients who are out of area early repatriation needs to be identified. Once the patient is ready the TTOs and discharge letter need completing. The referral to appropriate DGH is via the Orthopaedic Registrar on call. Please get accepting consultants name and document this in notes. Once this has been agreed inform nurse in charge of ward.
For repatriations back to Addenbrooke’s the registrar on call can accept them on behalf of the Consultant on call that day and they come under that consultant.
Useful information/phone numbers for those at Addenbrookes:
ACCOMMODATION
There are more than 500 rooms and flats available on campus for staff.
Doctors who wish to apply for accommodation need to contact the trust's medical staffing unit to obtain a security number for the online application form.
Sanctuary Housing manages this accommodation - Tel 01223 404800

Bedford Hospital is a 400-bed district hospital providing trauma and elective orthopaedic services. The department has 8 consultants which cover lower limb (hips&knees including soft tissue and revisions and foot&ankle), upper limb and paediatric conditions. All consultants have on-call duties. Spinal services are covered by Addenbrooke's.
There are 8 registrars, 2 of whom are regional trainees. Trainees rotate through a combined hip&knee rotation. The registrar on-calls include a mixture of resident (08:00-17:30) and non-resident (17:30-08:00) shifts. There is a team of Foundation Year 2 doctors covering the wards and the on-calls.
There are excellent opportunities for trainees to acquire surgical skills in routine orthopaedic trauma due to high numbers and availability of Consultants or experienced Senior Surgeons to supervise trainees.
Educational Supervisor: Mr Yadu Shankarappa
Princess Alexandra Hospital Harlow
|
Address: |
Hamstel Road Harlow CM20 1QX |
|
Phone: |
|
|
Founded: |
22 December 1994 |
|
Number of Beds: |
419 |
|
Educational Supervisor: |
Mr Satish Kutty, Mr Jehangir Mahaluxmivala |
|
Rota Co-Ordinator: |
Senior SPR |
|
Website: |
|
|
Trauma Coordinators: |
Nicola Edwards & Donna Ashcroft |
The Trauma & Orthopaedic Department in Princess Alexandra Hospital Harlow is a fantastic opportunity for specialist training, with multi- award winning orthopaedic consultants, friendly hospital staff, and great work ethics.
Rota
Consultant rota
In PAH the T&O Consultant on-call system is a daily on-call system:
-
12 Consultants do a fixed weekday (Mon-Thu) 1:3 rota and work 1:12 weekends (Fri-Sun)
-
The on-call day runs from 08:00 to 20:00
Emergency admissions are admitted under the care of the Consultant on-call at the time the referral is accepted. Spinal trauma is directed to Addenbrookes Hospital, and spinal cord emergencies are directed to Queens hospital. Open fractures and polytrauma are managed through the Major Trauma Network.
SpR/ Registrar rota
Each weekday (08:00 to 20:00, Mon-Thu) oncall will alternate between 3 registrars. The weekend (0:800 to 20:00, Fri- Thur) oncall will be a 1:12 rota. The Oncall Registrar will manage the oncall bleep and support the oncall junior doctor. A separate junior doctor will manage the admitted patients, preparing them for surgery or facilitating investigations. Our Trauma coordinators will assist in these duties, and arrange for admitting patients from home.
The on-call registrar for the night (20:00 to 08:00) will cover the Mon-Thu shift (Fri day off), or Fri-Sun shift (Mon-Tue days off). There is wonderful on-site accommodation available.
One registrar will attend the ward round on Saturday, and assist in the trauma theatre (08:00 to 17:00).
Consultants
The consultant firms:
|
Upper limb |
Ms Dimitra Leivadiotou |
|
Mr Rishi Dhir |
|
|
Hands |
Mr Simon Wimsey |
|
Arthroplasty & Revision arthroplasty |
Mr Charles Aldam & Paul Allen |
|
Mr Satish Kutty |
|
|
Mr Jehangir Mahaluxmivala |
|
|
Mr Dennis Kosuge |
|
|
Arthroplasty & Complex trauma |
Mr Unnikrishnan Ramkumar |
|
Arthroplasty & Soft tissue knee |
Mr Rashid Khan |
|
Foot & Ankle |
Mr Kar Teoh |
|
Spine |
Mr Mohamed Ahmed |
|
Mr Varadarajan Prakash |
|
|
Mr Arif Gul |
|
|
Paediatrics ortho |
Mr Dimitrios Manoukian |
2 SpR from East of England rotation
2 SpR from Potts rotation
2 SpR from Royal London rotation
2 SpR from Stanmore rotation
4 Staff grade Registrars
Clinics
Elective clinics are situated in PAH; St. Margaret’s Hospital, Epping; and Harts & Essex Hospital, Bishopstophard. Fracture clinics are based in PAH.Virtual fractures clinics are led by the consultants.
Theatres
Trauma theatre is run by one consultant for the week (Mon-Fri) and will have two registrars assigned each day. Elective lists will be located in main theatres or ADSU (day surgery).
Teaching
Each morning trauma meeting will consist of a multi-disciplinary meeting that includes the anaesthetic consultant, orthogeriatric consultant, physiotherapist and plaster technicians. All junior doctors must attend, as there will be teaching at all levels of orthopaedic knowledge. The FRCS exam candidates will have viva sessions.
The weekly evening registrar teaching has been organised by the department lead Mr Dennis Kosuge. The registrars organise a weekly teaching for the junior doctors during lunch time.
Monthly journal clubs are organised by Mr Simon Wimsey and frequently includes a well planned social night for the department.
Audit & Research
Ms Dimitra Leivadiotou is in-charge of audit projects, registrars should
Educational Supervisors
Mr Satish Kutty and Mr Jehangir Mahaluxmivala are Educational supervisors in PAH.
-
Formal meetings with your Clinical Supervisor(s): you should arrange initial, mid-point, and end-of-placement meetings: first month, third / fourth month and sixth month of each 6-month placement.
-
Formal meetings with your Educational Supervisor: please arrange a meeting at the beginning of each placement (to complete a learning agreement), and at the end of each placement, i.e. August, end-January or early February and June (before your ARCP in July).
-
You should achieve or be on track to achieve certain targets (or waypoints) to improve your chance of a successful outcome at your next ARCP. Further details are on the JCST website: www.jcst.org/quality-assurance/certification-guidelines
-
You should also keep your ISCP portfolio up-to-date, including uploading a current CV immediately prior to your ARCP.
The Queen Elizabeth Hospital, Kings Lynn
|
Address: |
Gayton Road Kings Lynn PE30 4ET |
|
Phone: |
01553 613613 |
|
Founded: |
1980 |
|
Number of Beds: |
515 |
|
Orthopaedic Tutor |
Mr James Jeffery |
|
Rota Co-Ordinator: |
Faye Chapman (Mrs). Direct line 01553 613952 |
|
Website: |
|
|
Trauma Coordinators: |
Sally Boswell (Mrs) & Mandy Manning (Mrs) |
The Trauma & Orthopaedic Department in The Queen Elizabeth Hospital is a fantastic opportunity for specialist training, with dedicated orthopaedic consultants, friendly hospital staff, and great work ethics.
Rota
Consultant rota
The Consultant on-call system is a weekly on-call system:
- 8 Consultants participate in a weekly on-call rota
- The on-call week runs 8-30am Mon – 8-30am Mon
Emergency admissions are admitted under the care of the Consultant on-call at the time the referral is accepted. Major trauma is directed to Addenbrookes Hospital through the Major Trauma Network. Spinal cord emergencies are directed to The Norfolk & Norwich Hospital.
Registrar rota
- 1 in 8 on call rota in conjunction with staff grade & associate specialist colleagues
- Protected teaching time for Regional Training Programme
- On call during the weekdays are for a 24 hour period, with a free morning after on call (weekdays only) to complete any duties required for the care of patients admitted during the previous 24 hours
- Weekend on call is for 48 hours (ie: Sat & Sunday), although mutually agreed & arranged (it is very important to involve the Orthopaedic Co-ordinator) splitting of Sat & Sun periods is allowed.
- On call is graded as ‘non-resident’. It is relatively unusual to be busy for any prolonged period at night & nigh time operating is the exception, rather than the rule as major trauma is usually diverted straight to Addenbrookes by the paramedic teams.
Consultants
|
Upper limb |
Miss Lucy Dennell & Mr Anil Chakrabarti |
|
Hands |
Mr Sunil Nair |
|
Revision arthroplasty (Hips) |
Mr James Jeffery & Mr Alan Norrish |
|
Knee Surgery (including revision arthroplasty & soft tissue reconstruction) |
Mr Siva Subramanian |
|
Foot & Ankle Surgery |
Mr Chandra Pasapula |
|
Primary Lower Limb Arthroplasty |
Mr Shantanu Mandal & Mr Mamoun Gadir |
|
Spine |
Mr Mamoun Gadir Mr Andrew Cook (N&N Cons; @ QEH alternate Mondays) Mr Nick Steele (N&N Cons; @ QEH alternate Mondays) |
|
Paediatrics |
Mr Rajiv Merchant (N&N Cons; @ QEH every Wednesday) |
Middle Grade Staff
- 3 ST trainees from The East Anglia Training Rotation
- 4 Staff Grade Surgeons (5th appointment pending)
- 1 Associate Specialist
Clinics
Elective clinics and fracture clinics are all held in the dedicated Orthopaedic Clinic department on the ground floor of the hospital near to the x-ray department. You should expect to have equal time allocated to fracture and elective clinics.
Theatres
• Trauma theatre is managed by the on-call Consultant for the week. Mondays & Saturdays are all day trauma lists. Tues, Wed, Thurs & Fridays are half day afternoon lists. There is no dedicated trauma list on Sundays. Case are discussed & scheduled at the 8-30am trauma meeting.
• Elective lists run all day Mon – Friday in main theatres. Allocation of theatre lists is made by the Orthopaedic co-ordinator usually 2-3 weeks ahead. In general ST’s should be mostly allocated to the lists working with the Consultant to whom they are attached. It is advisable to liase with the Orthopaedic co-ordinator in advance to arrange optimum individual list allocations.
Teaching
- The morning trauma meeting serves as an excellent teaching opportunity. Juniors of all grades gain confidence by presenting and discussing their management plans in this forum.
- Occasional journal clubs are scheduled (Mr Norrish has recently organised these with company sponsorship and a trip to a local restaurant afterwards). Historically it has proven difficult to coordinate teaching timetables with 3 Registrars as leave & timetabling conflicts have proven to be problematic.
- UEA & Addenbrookes Medical Students have attachments throughout the year in the Orthopaedic Department. Arranging teaching sessions for Med Students is wholeheartedly encouraged & well received. The Med Student teaching timetables are co-ordinated by Rob Golsby & Helen Bensley, who are based in the Undergraduate Department of the hospital, near the entrance to theatre changing rooms.
Audit & Research
Mr Chandra Pasapula is the lead for audit projects. Mr Pasapula has an excellent track record of publications over the last decade. He encourages Registrar involvement in his projects, many of which have had an anatomical bias.
During the 12 month attachment at The QEH each Registrar should aim to complete and present a project which they have lead. The best forums are CTOC – Cambridge Trainee Orthopaedic Club & EAOC – East Anglia Orthopaedic Club Meetings, usually held in March & November (Covid permitting). All Consultants should be able to suggest projects, but it is expected that the trainee demonstrates initiative to conduct & complete such audit/ research projects.
Consultant Supervisors
Mr James Jeffery is the Educational Supervisor/ Orthopaedic Tutor at
QEH.
Please arrange a meeting at the beginning and end of each placement to complete a learning agreement. Ensure that the sign off is completed before your ARCP in July.
Registrar allocation is Team Based. The pairings are:
Mr Jeffery & Mr Nair
Mr Subramanian & Mr Pasapula
Miss Dennell & Mr Gadir
Either Consultant of each pair can act as a Clinical Supervisor, this will be decided at the induction meeting. The new MCR (Multiple Consultant Report) in fact means that all Consultants whom you have exposure too will be involved in preparing a report on your progress.
There is plenty of scope outside these pairings to attend lists with all other Consultants & this is encouraged, especially during the times when an allocated Consultant may be on leave.
Please arrange initial, mid-point, and end-of-placement meetings with your Clinical Supervisor.
- You should achieve or be on track to achieve certain targets (or waypoints) to improve your chance of a successful outcome at your next ARCP. Further details are on the JCST website:
www.jcst.org/quality-assurance/certification-guidelines
- You should also keep your ISCP portfolio up-to-date, including uploading a current CV immediately prior to your ARCP.
Peterborough City Hospital
| Address: | Peterborough City Hospital, Edith Cavell Campus, Bretton Gate, Peterborough, PE3 9GZ |
| Phone: | 01733 678000 |
| Founded: | 1937 |
| Number of Beds: | 612 |
| Educational Supervisor: | Mr Andrew McKee |
| Rota Co-Ordinator: | Anne Uddin anneuddin@pbh-tr.nhs.uk Ext 7176 |
| Website: | https://www.peterboroughandstamford.nhs.uk |
| Human Resources: | Andrea Brown. andrea.brown@pbh-tr.nhs.uk Ext 7854 |
| Trauma Co-Ordinator | Sue and Gemma - Ext 8711 |
Orthopaedic Department
Peterborough City Hospital offers a busy elective and trauma service. There are 16 Consultants. The elective and trauma placements are separated. Trainees are expected to rotate either 4 or 6 months through trauma and then elective services.
There are 5 orthopaedic theatres which run every day – 4 elective and 1 trauma theatres. There is a full day dedicated trauma list everyday, including Saturday and Sunday which is run by the consultant oncall.
The weekends are staffed by 2 registrars, one covers the oncall and does not attend theatre and one who purely covers the trauma list.
There are excellent opportunities for trainees to acquire sub-specialty skills. Areas which have received excellent trainee feedback include the shoulder firm, hand firms, foot and ankle firms, paediatrics and lower limb arthroplasty. There is no spinal service.
Rota:
A shift system is in place with 24 hour non-resident on-call shifts and 48 hour weekend shifts.
Theatres and Clinics:
An average week for trainees includes:
- 2 elective (sometimes more!) and 1 fracture clinic,
- 1 ½ – 2 full day elective or trauma theatre with respective consultant,
- 1 half day research/CME session.
- Protected Thursday afternoon for SPR teaching.
Firms:
- Mr White and Mr Jones – Shoulders and Hands
- Mr McKee and Mr Pathak – Hand and Elbow
- Mr Clifton and Mr Hartley – Lower limb arthroplasty and soft tissue knee
- Mr Reston and Mr Chowdhury – Hip and revision hip arthroplasty
- Mr Carmichael and Mr Kamath – Foot and Ankle
- Mr Latimer and Mr Mitchell – Paediatrics
- Mr Heinert and Mr Massraf – Lower limb arthroplasty
- Mr Parker – Hip fractures
Teaching and Training:
Teaching sessions include a trauma meeting every morning, Tuesday lunchtime teaching run by the registrars and a Friday metalwork meeting.
Every month or so there is an evening workshop organised with industry representatives to provide saw bone sessions for new registrars and familiarise yourselves with the systems used the hospital. This usually includes a dinner afterwards.
Medical students:
The hospital receives medial students from both Leicester and Cambridge medical schools. The students become very involved in the department and give excellent feedback.
There is a registrar led teaching program which is highly regarded by the medical students who rotate through Peterborough.
James Paget
- 458 beds
- 26 day case beds
- Spinal referrals discussed with Norwich
We are:
- 10 Consultants
- Specialist Associates & middle grades
- Visiting consultants- Spines- Mr Lutchman & Mr Swarmy; Paediatrics- Mr Sanghrajka
Key Contacts
Address: Lowestoft Road Gorleston-on-Sea, Great Yarmouth NR31 6LA. Tel: 01493 452452
Educational Supervisor: Mr Sunil Garg
Rota Co-ordinator: Mr Nitin Modi
https://www.jpaget.nhs.uk/about-us/
The team
- 1 trainee
- 1 MTS
- 7 SAS/ Middle grades
|
Specialty |
Consultant |
|
Upper limb |
Mr Garg Mr Modi |
|
Lower limb- Hips |
Mr Cohen Mr Nakhla Mr Nnene Mr Rathi |
|
Lower limb- Knees |
Mr Deo Mr Khurana Mr Cutts |
|
Lower limb- Foot and ankle |
Mr Devaney |
Rota
Consultants rotas is across one week (Friday-Friday) and is a frequency of 1 in 9. This begins at 8am and finishes at 8am the following week. As a registrar, you will be on-call with your consultant during this week and due to the hours at the weekend, this will be divided up.
Outside of the on-calls, there will be scheduled out of hour on-calls across the other 8 weeks as stand alone nights.
Structure of On-call day:
8:00- Trauma meeting (on Microsoft teams)
9:00- Ward round
10:30-12:30- On-call fracture clinic
13:00- Trauma Theatre
17:30-18:00- Check admissions and handover to OOH team
All referrals and admissions during this period will belong to that consultant team. During the on-call week, theatre sessions in the morning are scheduled for trauma patients but operating will be timetabled by other teams. During the weekend, you will be non-resident on-call and a junior doctor specially covering orthopaedics will cover the bleep until handover the following day. You will be expected to attend during the on-call out of hours if required.
Normal Week
During a normal week, there will be scheduled elective theatre, clinics, fracture follow up clinics and trauma theatre sessions. It will be expected to cover your teams ward patients during this time.
Teaching
From 12:00-13:00, lunchtime meetings will be held most regularly throughout the week on Zoom. These are a mix of teaching, focus meetings and departmental teaching. Due to the frequency and with timetable constraints, it is understood that not every meeting is relevant or possible to attend but this is encouraged. Regional teaching attendance is encouraged. To accommodate this rota co-ordinators, need to be contacted early.
The spinal team will visit each Thursday for elective theatres and clinics. Mr Sanghrajka visits for Paediatric clinic every week with 1 in 4 weeks this is converted to a theatre list. You are welcome to attend these clinics- please let rota co-ordinators know in advance and liaise with respective consultants.
Annual Leave
This should be emailed into the respective consultants’ secretary, Consultant and Mr Modi. This should be at least 6 weeks in advance to adjust elective commitments.
Study Leave
A paper form needs to be completed for leave, available from the Post graduate medical centre (PGMC). This should 6 weeks prior to the date. Again, this should be communicated with your consultant and admin team.
Regional teaching will always be accommodated but please email dates for this as early as possible.
Research and Audit
The department welcome involvement with audits and research. There are many opportunities to get involved with these for both local and national projects.
Theatres
Theatre 1&3 - Trauma
Theatre 4- Elective
Theatre opportunities
There will be opportunities to operate with your consultant for trauma, both during and outside the on-call. There will also be scheduled elective theatre opportunities. Outside of these times, you are encouraged to join other operating lists if your schedule allows.
Wards
- 6- General Orthopaedic trauma
- 22- Outlier Orthopaedics trauma
- Charnwood/ Day Surgery Unit- Electives
Comments
This is the newest hospital to join the region and capacity of trainees to work in the department is likely to change over time. Due to specialist clinics and volume of trauma this is a good training placement.

