Medical psychotherapy higher training in the East of England is offered through dual training with General Adult Psychiatry.
The five year advanced training enables qualification on the GMC specialist register with two Certificates of Completion of Specialist Training (CCT) as a Medical Psychotherapist and as a General Psychiatrist.
"I chose dual training in general psychiatry and medical psychotherapy because I was interested in understanding mental health and illness in a broad manner. I wanted to learn to draw on different models to understand patients' difficulties, including biological/organic, psychodynamic, cognitive-behavioural and systemic explanations. I value this because it allows greater insight, depth and creativity in working with patients.I have valued learning to work in a way that seeks an understanding of the patient's internal world and the meaning of the difficulties that they experience. I have found that placing the clinician-patient relationship at the centre of what I do, and thinking in detail about my experience of the patients I work with, has enriched my work as a psychiatrist."Charles le Grice, ST6 dual trainee
|
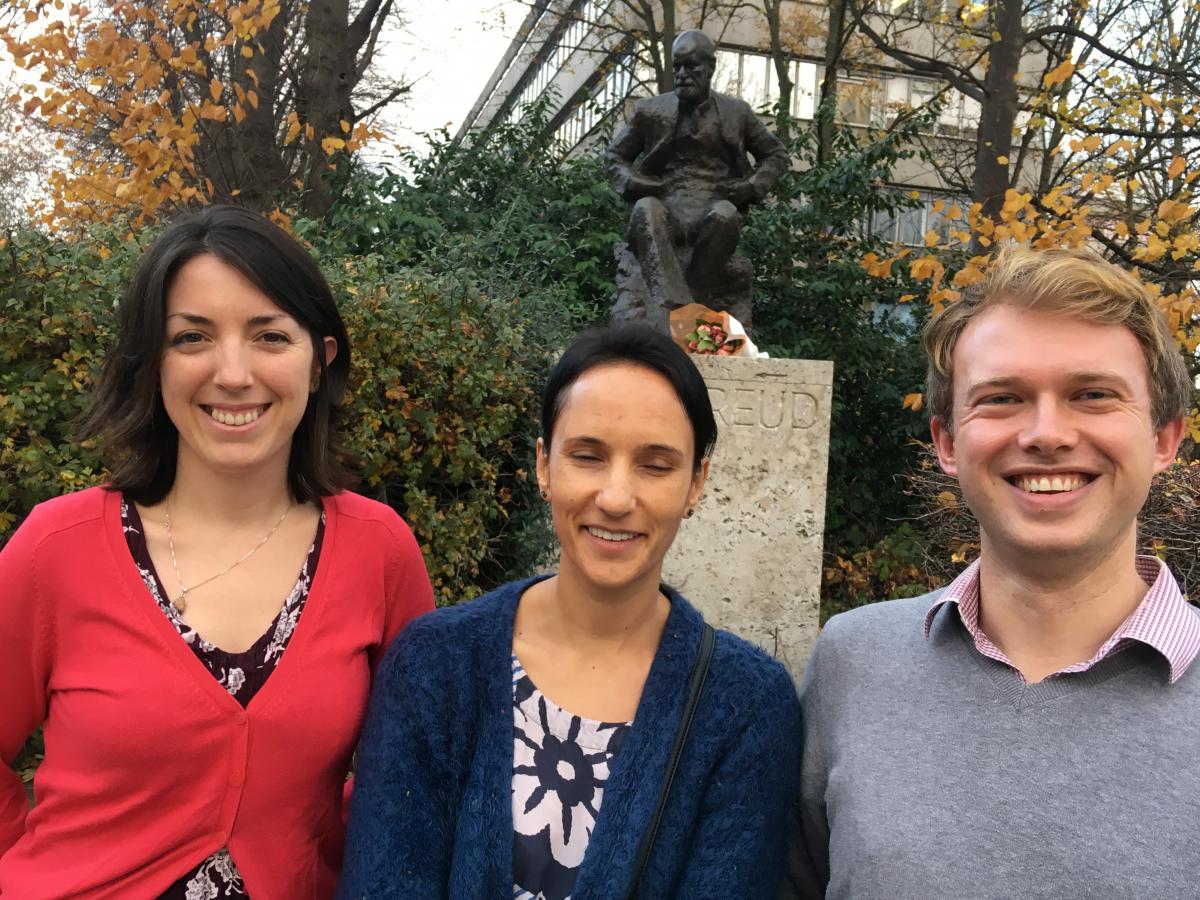
Dr William Burbridge-James
Dr David Middleton |
|
Training Programme Director East of England Higher training in Medical Psychotherapy; Psychotherapy Tutor; Consultant Psychiatrist in Medical Psychotherapy; Head of Complex Needs Personality Disorder & Psychotherapy Services South Essex; Chair of Specialty Advisory Committee, Faculty of Medical Psychotherapy RCPsych william.burbridge-james@nhs.net
Training Programme Director East of England Higher Training in General Adult Psychiatry |
|
Dr Anna Crozier |
|
ST4 dual trainee Medical Psychotherapy/General Adult Psychiatry Essex Partnership NHS Foundation Trust |
|
Dr Jessie Ke |
 |
ST4 dual trainee Medical Psychotherapy/General Adult Psychiatry, Essex Partnership University NHS Foundation Trust |
 The national and regional perspective over the last few years has led to the development of dual training programmes combining Medical Psychotherapy and General Adult Psychiatry. Since the introduction of dual training, medical psychotherapy appears to be thriving. This five year training programme was ratified by the General Medical Council in 2012. Benefits of dual training include reducing the time needed to learn both specalities, increasing trainees' empoyability and personal choice.
The national and regional perspective over the last few years has led to the development of dual training programmes combining Medical Psychotherapy and General Adult Psychiatry. Since the introduction of dual training, medical psychotherapy appears to be thriving. This five year training programme was ratified by the General Medical Council in 2012. Benefits of dual training include reducing the time needed to learn both specalities, increasing trainees' empoyability and personal choice.
The training programme is guided by an awareness of the need for the future Consultant Psychiatrist in Medical Psychotherapy/General Adult Psychiatry to deliver expert psychotherapy and also apply expert psychotherapeutic thinking to inform patient care through consultation and reflective practice in a range of psychiatric settings. Combining psychiatric an psychotherapeutic clinical skills can improve the quality of patient care, particularly in areas where these combined skills can be used in work with complex and severe mental health difficulties.
This dual training offers a psychotherapeutic approach to the understanding of human personality development, which forms a bridge between both the general psychiatric and the general psychotherapeutic patient populations. The dual training will also orientate itself to incorporating a developmental perspective for the trainee, to equip them to understand and respond to the emotional demands of working in general psychiatric settings therapeutically.
In the Eastern deanery the major model of therapy is psychoanalytic psychotherapy and for trainees personal therapy will be a central required part of their professional development throughout the five year training programme.
The importance of an awareness of a range of models of psychotherapy is incorporated in the dual training programme in line with the Royal College of Psychiatrists’ curriculum requirements for medical psychotherapy training.
In addition, the role of pharmacotherapy in combination with psychotherapy is a feature of both the psychiatric and the medical psychotherapeutic training of the dual trainee, who will be using psychotherapeutic approaches (alongside psychotropic medication and psycho-bio-social approaches)
 The dual training is five years in length and trainees are currently based in Essex Partnership University Foundation Trust.
The dual training is five years in length and trainees are currently based in Essex Partnership University Foundation Trust.
On satisfactory completion training leads to the award of two Certificates of Completion of Training (CCT) in Medical Psychotherapy and General Psychiatry. The dual trainee will at all times be allocated an educational supervisor (trainer) who is a trained Consultant Medical Psychotherapist and an educational supervisor (trainer) who is a Consultant General Psychiatrist.
There are three strands to the training programme over the five years. One strand is a full higher training in General Psychiatry, the second strand is a full higher training in Medical Psychotherapy and the third strand is in integrating these two sub-specialty trainings in the applications of psychotherapy in different psychiatric settings.
Year 1&2 - ST4 and ST5
Three days per week will be spent in General Adult Psychiatry which may begin in any General Psychiatry setting, with in-patient teams often favoured over a community mental health team to begin. The General Adult Psychiatry Educational Supervisor is the Consultant in this setting. During this time trainees are expected to use the special interest/research sessions for psychotherapy. Trainees will begin the academic component of their psychotherapy training and will be expected to attend an appropriate training course in psychoanalytic theory and currently the scheme has relationships with the Tavistock clinic in London. Trainees will also begin to see psychotherapy cases. Clinical supervision of psychotherapy cases seen once weekly will begin in the first year and continue throughout the training. The trainee’s Medical Psychotherapy Educational Supervisor will remain their trainer beyond the first two years of the training to provide continuity and containment.
Year 3&4 – ST6 and ST7
The trainee will be in the Psychotherapy post based in North or South Essex. Special interest session alongside on-call commitments maintain the links to general adult psychiatry during these years. Trainees continue their academic and clinical training links with the appropriate training courses. Trainees have the opportunity of gaining experience in other psychotherapy teams both within Essex and as part of external academic training courses.
Year 5 – ST8
The final fifth year of dual training (ST8) focuses on building on the integration of the two sub-specialities of Psychotherapy and General Psychiatry in line with the trainee’s career aspirations and training needs. Trainees also have the opportunity to achieve leadership competencies in this year.
Further information about the Higher Specialty Training in General Adult Psychiatry in Essex Partnership University Foundation Trust can be found here.
The trainee is expected to gain clinical psychotherapy experience and achieve competencies in a range of domains. This includes provision of therapy in their primary and supplementary modalities; carrying out assessments for psychotherapy and offering psychotherapeutically informed consultations on complex cases to other specialist colleagues.
In order to achieve their competencies, it will be expected that the trainee will carry out approximately 60 hours of assessments, 700 clinical hours in their adopted major model of psychotherapy and 100 clinical hours in two supplementary models of therapy, which can include supervision.
The three models will be chosen from psychoanalytic psychotherapy (the primary model in the East of England deanery), cognitive behavioural therapy/DBT and systemic therapy. The Training Programme Director will decide with the trainee and Medical Psychotherapy Educational Supervisors what clinical experience and models of psychotherapy can contribute to the hours of experience required.
Clinical Supervision
The dual trainee will receive clinical supervision from practitioners both within the scheme in psychotherapy and also outside of the scheme as part of their external academic training. Supervision will take place of work in primary and supplementary modalities.
In the early stages of training (ST4, ST5) clinical supervision is primarily from the Consultant Psychiatrists in Psychotherapy who have a Medical Psychotherapy CCT and who are trainers in the Medical Psychotherapy Training Programme.
Later in training (ST6 onwards) clinical supervision is sought from other professions with a registered training in the chosen model of psychotherapy.
Clinical supervisor’s reports will be requested from supervisors in primary and supplementary modalities on a once yearly basis around six months before the Annual Review of Competence Progression (ARCP). These Clinical Supervision Reports will be used to inform the annual assessment of the trainee’s progress and development for the Annual Psychotherapy Appraisal between the Trainee, Medical Psychotherapy Educational Supervisor and Training Programme Director prior to and in preparation for the Annual Review of Competence Progression (ARCP).
Work place based assessment of all psychotherapies will be undertaken, including the formative Structured Assessment of Psychotherapy Expertise (SAPE) during clinical supervision of therapy, Structured Assessment of Psychotherapy Assessment (SAPA) and a summative Psychotherapy Assessment of Clinical Expertise at the end of each therapy (PACE or Psychotherapy ACE). Work place based assessment (WPBA) of consultation will include cased based discussion (CBD) Structured Assessment of Psychotherapy Expertise (SAPE) and Assessment of Clinical Expertise (ACE). All these WPBAs are on line in the Royal College of Psychiatrists’ portfolio on line training website. The Work place based assessment (WPBA) Direct Observation of Non-Clinical Skills (DONCS) can be used for chairing professionals meetings or participating in a Care Programme Approach meeting as part of the ‘consultation sandwich’ approach developed in by colleagues in Leeds. The consultation sandwich includes seeing the professionals, then sometimes seeing the patient, then seeing the professionals again to formulate and offer recommendations on on-going patient care and management.
All trainees will be required to maintain reflective practice reports discussed in Educational Supervision of their psychotherapies and general psychiatry assessment feedback as part of self-reflective practice development in the Advanced Medical Psychotherapy Curriculum (2013)
The clinical supervisors who supervise the clinical work within the scheme are invited to attend and contribute to the Deanery Medical Psychotherapy Training Committee to facilitate the development of the Medical Psychotherapy Training Scheme.
Trainees undertaking psychoanalytic training undergo their own personal analytic experience to think about the impact of the work with severe psychiatric disturbance, and in particular the emotional challenges of working across different settings with potentially very different ways of thinking about patients.
Psychoanalytic psychotherapy is required throughout the training period with a psychoanalyst or a psychoanalytic psychotherapist registered with the British Psychoanalytic Council and agreed with the Medical Psychotherapy Training Programme Director. The trainee may begin in a once weekly therapy and increase the frequency as they develop through the training. It is expected that personal therapy would continue throughout the duration of training.
Funding for personal therapy is provided by the Deanery for Medical Psychotherapy Trainees in for one session of personal psychotherapy or psychoanalysis
Teaching, Training and Supervising
Towards the mid part of the training (ST4-ST6) the dual trainee will be actively involved in teaching, training and supervision. This will include the provision of clinical case supervision to Core Trainee Psychiatrists (CT1-CT3) and lectures on the post-graduate education programme. The trainee will develop and evaluate teaching materials and develop medical education competencies.
The clinical supervision of Core Trainee Psychiatrists undertaking the brief and longer term psychotherapy cases to fulfil the psychotherapy training curriculum of the Royal College of Psychiatrists will be complemented by the trainee joining a supervision of supervision group for supervisors in the department in Southend.
The dual trainee will also have an opportunity to observe a Consultant Psychiatrist in Psychotherapy conducted Balint group for Core Trainee Psychiatrists and will later in training (ST6 onwards) facilitate their own Balint group, for undergraduates, Foundation doctors and Core Trainees. The dual trainee is required to conduct work place based assessment of their Balint groups using the Balint group assessment (CBDGA) and formative assessment of their clinical supervisees using the Structured Assessment of Psychotherapy Expertise (SAPE).
The dual trainee will also maintain reflective practice reports discussed in Educational Supervision of their Balint group feedback and clinical supervision experience as part of self-reflective practice development in the Advanced Medical Psychotherapy Curriculum (2013).
Reflective Practice
One important role for the application of medical psychotherapy skills lies in supporting the development of reflective practice competence amongst colleagues.
The dual trainee will observe and participate in reflective practice groups facilitated by a Consultant Psychiatrist in Psychotherapy in the early part of training (ST4 and ST5) and from mid training onwards will use consultation activity to develop reflective practice competence in others.
Consultation and reflective practice supervision provided by a Consultant Psychiatrist in Psychotherapy will provide a foundation for the dual trainee from ST6 onwards to bring consultations observed and seen and for the dual trainee to plan and establish running a reflective practice group in an acute psychiatric setting such as an in-patient ward or a crisis team. The dual trainee would not be expected to consult with colleagues within their General Psychiatry placement as this would place them in the dynamic of an internal consultancy position making this untenable.
The dual trainee will also maintain reflective practice reports discussed in Consultation and Reflective Practice Supervision of their consultation and reflective practice activity experience as part of self-reflective practice development in the Advanced Medical Psychotherapy Curriculum (2013).
The aim of the dual training programme is to help the trainee to become a medical psychotherapist and psychiatrist, who embraces and integrates their medical and psychiatric identity as a specialist psychotherapeutic psychiatrist. The general goals of professional attributes, risk, audit, teaching and supervision, clinical and service management, organisational change and clinical governance form the backbone of this training programme as they do other advanced psychiatric training programmes.
 The distinct theoretical and experiential aim of dual training is to integrate the knowledge and skills of two CCT trainings in both General Adult Psychiatry and Medical Psychotherapy in such a way that the future Consultant Psychiatrist in Psychotherapy is helped to inform their professional orientation to their Medical
The distinct theoretical and experiential aim of dual training is to integrate the knowledge and skills of two CCT trainings in both General Adult Psychiatry and Medical Psychotherapy in such a way that the future Consultant Psychiatrist in Psychotherapy is helped to inform their professional orientation to their Medical  Psychotherapy role according to these two different sub-specialities and different paradigms of mind.
Psychotherapy role according to these two different sub-specialities and different paradigms of mind.
Psychoanalytic trainees will be required to learn about the theoretical foundations of Psychoanalytic Psychotherapy. There are existing links with courses in the Tavistock. Trainees apply separately for places on these courses usually at the beginning of the 5 year programme and are encouraged to attend during their special interest sessions.
There are various options which would fulfil the theoretical component of the training programme. The Foundations of Psychodynamic Psychotherapy course (previously D58) at the Tavistock would meet the requirements of the first two years of dual training. Trainees may wish to continue this Diploma course into a third year to write a dissertation and obtain a Master’s degree and we would support this.  Psychoanalytic trainees may consider and discuss the possibility of an external psychoanalytic training with a training recognised by the British Psychoanalytic Council during their training in developmental discussion with their Medical Psychotherapy Educational Supervisor, such as the Tavistock (MI) Interdisciplinary Training in Adult Psychotherapy. However, while application for external psychoanalytic training may occur within the dual training it is often the case that such training cannot commence until the trainee has completed their Consultant Psychiatrist in Psychotherapy training and is established geographically in post so the time commitment of training (usually five years) can be successfully completed.
Psychoanalytic trainees may consider and discuss the possibility of an external psychoanalytic training with a training recognised by the British Psychoanalytic Council during their training in developmental discussion with their Medical Psychotherapy Educational Supervisor, such as the Tavistock (MI) Interdisciplinary Training in Adult Psychotherapy. However, while application for external psychoanalytic training may occur within the dual training it is often the case that such training cannot commence until the trainee has completed their Consultant Psychiatrist in Psychotherapy training and is established geographically in post so the time commitment of training (usually five years) can be successfully completed.
The Dual Medical Psychotherapy and General Psychiatry Training Programme will aim to help the trainee to integrate any external psychoanalytic training with their development as an NHS Consultant if they are accepted and commence training within the CCT training period.
Audit
The trainee will be expected to have an understanding of the audit cycle and carry out at three-four audit projects during their training in Medical Psychotherapy and General Psychiatry.
Research
The trainee will be expected to familiarise themselves with the literature in relation to the evidence base and research in their respective sub-specialties. The methodological strengths and weaknesses of the relevant literature should be familiar.
The issues surrounding the evidence base and comparison between different models of psychotherapy should be familiar. The trainee should be aware of current psychotherapy outcome measures and their strengths and limitations and should be able to appraise the literature critically.
The dissertation for the Interdisciplinary Training in Adult Psychotherapy (M1) or Foundations of Psychodynamic Psychotherapy D58 course may be used as the basis for a research paper.
Management
The dual trainee will attend the Psychological Services Senior Management Group Meeting in EPUT or other committee meetings during their placements to compare the different ways teams and Trusts work and to observe the different organisational contexts and their influences. Trainees are encouraged to apply to courses in leadership and management such as those provided by the deanery, LEAP and Chief Residents' Programme. Trainees may gain further relevant experience by acting as trainee representatives to groups at Trust and Deanery level.
A clinical governance perspective on psychotherapy service delivery including the economic aspects of care systems will be incorporated throughout the programme.
The trainee will be expected to attend Deanery and national management courses at points in their training which are relevant to their needs.


