East of England Anaesthetics ARCP GUIDE
Please also see the RCoA ARCP checklists which are available by clicking here.
Abbreviations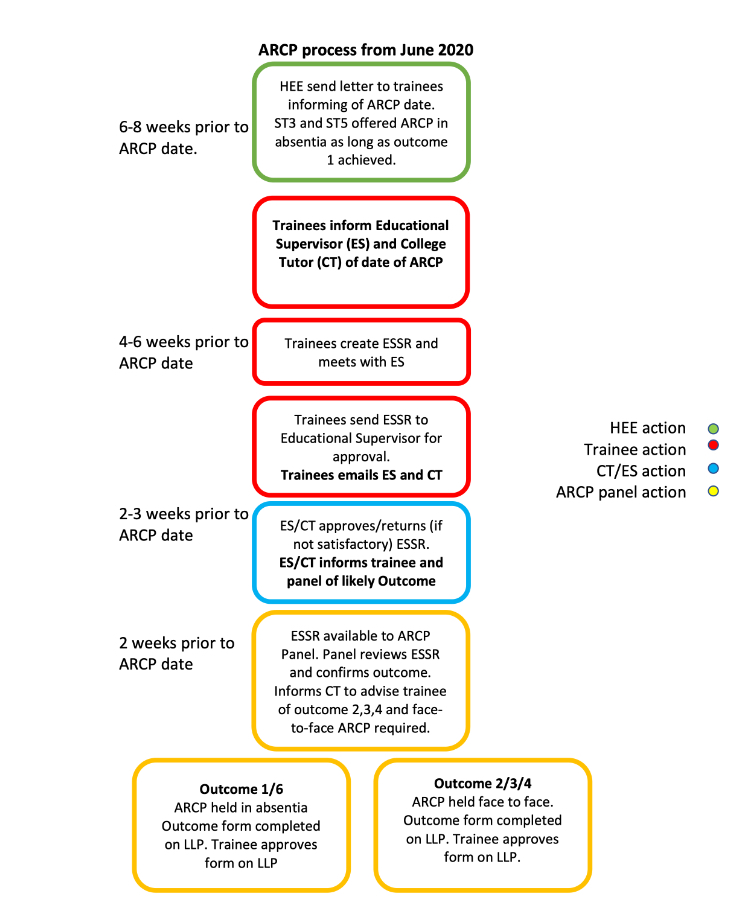
|
ARCP |
Annual Review of their Competency Progression |
|
EoE |
East of England |
|
ICM |
Intensive Care Medicine |
|
CCT |
Certificate of Completion of Training |
|
LTFT |
Less Than Full Time |
|
HEE |
Health Education England |
|
CT |
College Tutor |
|
ES |
Educational Supervisor |
|
ESSR |
Educational Supervisors Structured Report |
|
HALO |
Holistic Assessment of Learning Outcomes |
|
IAC |
Initial Assessment of Competencies |
|
IACOA |
Initial Assessment of Competencies in Obstetric Anaesthesia |
|
EPA |
Entrustable Professional Activities |
|
CCC |
Completion of Capability Cluster |
|
GPC |
Generic professional Capabilities |
|
SIA |
Special Interest Area |
|
SLE |
Supervised Learning Events |
|
MTR |
Multi Trainer Report |
|
MSF |
Multi Source Feedback |
|
CESR(CP) |
Certificate of Eligibility for Specialist Registration (Combined Programmed) |
|
OOP (E/T/R/P) |
Out Of Programme (Experience/Training/Research/Pause) |
All trainees within the anaesthetic and ICM training programmes are required to undertake an Annual Review of their Competency Progression – the ARCP - every year.
How will I know when my ARCP is?
You will be notified by email at least 6 weeks before the date of your ARCP:
- August starters: you should expect to have your ARCP in June or July.
- February starters: yours will usually be in January.
- Final ARCP at ST7: around 3 months prior to CCT date, usually May or November
- LTFT with finish dates out of sync with Feb and August: you will need an ARCP within 3 months of your CCT date and this may be shortly after a June or January ARCP.
All LTFT trainees will also be required to have 12 monthly ARCPs. This is not pro-rata and therefore you will have more ARCPs during your training than a full-time trainee.
If you are going on Maternity Leave you may be asked to have an ARCP before you go on maternity leave so summarise your training to that point and help to complete the SuppoRRT documentation prior to going on Maternity Leave.
All ARCPs will be in ABSENTIA unless a non-standard outcome is expected – i.e. Outcome 2, 3, or 4.
Once you receive the invitation from HEE please inform your College Tutor (CT) and Educational Supervisor (ES) of the date. The CT and ESs do not get informed of these dates. It is important to plan your ES meeting to complete your ESSR and be aware of holiday dates for your ES and CT so that there is no last-minute rush. An ESSR can be prepared before you get your invitation.
Your ESSR should be available for the panel to view 14 days before the date of your ARCP. This allows time for the panel to assess the ESSR prior to the ARCP.
The panel can only assess evidence attached to the ESSR therefore please ensure you attach all the evidence of your progress over the year including evidence of teaching, research, quality improvement and leadership activities.
What evidence do I need to provide before my ARCP?
We follow the RCOA guidance for ARCPs for all trainees on the 2010 curriculum.
For trainees on the 2021 curriculum we are awaiting full guidance from the RCOA. In the meantime you should provide evidence of progress towards and achievement of the Key Capabilities and HALOs. We would not expect you to have the HALOs completed until the end of your stage of training.
|
ACCS (CT2) Stage 1.2
|
IAC, EPA 1+2 and SEDATION HALO Completed all 11 learning outcomes from ACCS curriculum Demonstrate progress in GPC domains and other HALOs. Please refer to the ARCP decision aid on the ACCS website: https://www.accs.ac.uk/ |
|
Stage 1.1 Core anaesthesia (CT1) |
IAC, EPA 1+2 and SEDATION HALO Demonstrate progress in GPC domains and other HALOs. |
|
End ACCS (CT3) Stage 1.3 Stage 1.2 Core anaesthesia (CT2) |
IACOA EPA 3 + 4 Demonstrate progress in GPC domains and other HALOs. |
|
End ACCS stage 1.4 (CT4) End Core anaesthesia Stage 1.3 (CT3) |
All remaining HALOs Completion of Primary FRCA exam. |
|
Stage 2.1 (ST4) |
Demonstrate progress in most areas of the GPC domains and good progress in other HALOs. CCC in Paeds/ Obs/ Cardiac or Neuro if these units are done in this year. |
|
Stage 2.2 (ST5) |
Completion of all CCC’s and all HALOs Completion of Final FRCA |
|
Stage 3.1 (ST6) |
Demonstrate progress towards all GPC domains and the general Stage 3 HALOs. Completion of Special Interest Area (SIA) domains done in this academic year |
|
Stage 3.2 (ST7) |
Completion of all Stage 3 HALOs and SIA units. |
ESSR
Before opening the ESSR please ensure your profile is up to date, your exam passes are updated and your placements are correct.
Any documents you wish to use to use to evidence your progression should be uploaded as a Personal Activity under an appropriate heading on the LLP and should marked as visible in the ESSR.
- Educational Supervisor’s Structured Report (ESSR) - labelled ARCP (year, date) ESSR which should be completed and available 2 weeks to the ARCP panel before the ARCP date. This means that it has been reviewed and approved by both your Educational Supervisor and the College Tutor before 2 weeks before your ARCP date.
- The ESSR should be generated for the dates from your last ARCP. This will pull in all the data for the whole year including interim ESSRs.
- The ESSR should include the following:
- An interim ESSR for each placement such as the cardiac and neuro units of training summarising the time spent in the 3 months attachment. On 2021 curriculum use the Completion of Capability Cluster (CCC) for cardiac, neuro, paeds and obs for these blocks.
- EM/AM placements for ACCS CT1 and any 6 months extensions.
- An Interim ESSR will also need to be done if a trainee is moving trust in the middle of the year (replaces old intermediate progress reports)
- Evidence of progress with Modules/ Domains, using WPBA/SLEs, reflections and other suggested activities uploaded onto LLP.
- RCOA logbook summaries for the year being reviewed (The 12 months prior to the ARCP will be reviewed). You will need filtered logbook summaries for neuro, cardiac, obs and paeds to complete the CCC.
- Exam attempts and their outcome. Ensure you update the profile with your exam pass dates.
- MSF - should be closed and send to educational supervisor minimum 3 weeks before the ARCP date. This needs to be reviewed and released by the ES for it to be visible on the ESSR.
- An additional MSF is required for ICM if completed during the period under review.
- Consultant Feedback/ Multi trainer report (MTR) – now to be completed via the LLP and sent out by your College Tutor. You need one per year as well as one for the IAC and IACOA, and one for each CCC (Paeds, Obs, Cardiac and Neuro)
- For ACCS CT2 trainees you require an MTR for Anaesthesia and an MCR for ICU
- Check your milestones are visible – IAC, IAOC, Stage certificates.
- Any courses/simulation training/meetings attended
- Audit/Quality improvement activity
- Any research undertaken (academic trainees need to also complete the separate academic training report sent by HEEoE)
- An up-to-date CV
- Any compliments - anonymised
- Any incidents/complaints and associated reflection – ensure this is recorded under incidents on the ESSR by your ES
- An up-to-date Personal Development Plan.
- Educational Supervisor meeting – a minimum of 3 per year. Either upload a pdf/jpeg of the meeting summary or complete a meeting summary on the LLP.
- ACCS trainees require an end of placement report for each placement, uploaded to their LLP, available here: https://www.accs.ac.uk/new-and-events
What is the FORM R?
Information about the form R is available on the revalidation and assessment section of the HEEoE website. This link shows you how to electronically sign your Form R.
You do not need to list all the rotations you have had prior to this ARCP. You only need to list the rotations relevant to your current ARCP.
If you have been involved in an incident it will need to be recorded on the Form R AND under incidents on the ESSR. It will need to be discussed with your ES and reflected upon. Please see below on how to reflect up on an incident. If you have uploaded a reflection on your LLP. Please indicate on the Form R the date and where on the LLP you have uploaded the reflection.
Email the completed Enhanced Form-R document to HEEoE THREE WEEKS before your ARCP: THEN Upload to your LLP as a personal activity labelled FORM-R and assign to your ARCP year 2 weeks before your ARCP date.
When do I need formal Consultant Feedback(CBF)/Multi Trainer Report (MTR)?
Listed below are the timescales when we would like to see written Consultant feedback now called Multi Trainer Report (MTR) on the LLP. This will need to be generated by the College Tutor. Consultant feedback differs from MSF as it concerns a trainee’s progress in a specific domain of training only. MSF seeks feedback from the multidisciplinary team, including consultants, on overall professional behaviour. The MSF and MTR can be used as evidence to support achievement of Learning Outcomes for the GPC HALOs. In ACCS ICU it is called the Multiple Consultant Report (MCR).
Stage 1
3 months (to inform IAC)
One to inform IACOA
MTR if doing a CCC for obstetrics and paediatrics
Otherwise one MTR per year
For ACCS CT2 trainees you require an MTR for Anaesthesia and an MCR for ICU
Stage 2
At the end of Neuro, Cardiac, Paeds, and Obs to inform sign off of CCC and to all Consultants prior to ARCP at ST4 and ST5
Stage 3
At a minimum of one a year but also for each Special Interest Area completed.
Who will be on the panel?
The panel will be made of representatives from Health Education East of England and the School of Anaesthesia. There may also be a lay member and/or an external member representing the College (assessing the panel rather you). Your Educational Supervisor is not usually a member of the panel but may come along to support you in some instances.
There will be a military member or academic member if you require this representation.
What are the possible outcomes?
The possible outcomes are detailed on the assessment and revalidation section of the HEEoE website.
You should all be aiming for an Outcome 1 apart from:
- CT2's (Core Anaesthesia 2010 curriculum) CT3’s (ACCS Anaesthesia 2010 curriculum) or at the end of Stage 1 (2021 curriculum) and ST7's - where you are completing the training program and will hopefully be awarded an outcome 6.
Possible outcomes are:
- Outcome 1 - Satisfactory progress - achieving progress and the development of competencies at the expected rate.
- Outcome 2 - Development of specific competencies required - additional training time not required
- Outcome 3 - Inadequate progress - additional training time required (extension of anticipated core training programme end date or anticipated CCT/CESR(CP) date
- Outcome 4 - Released from training programme - with or without specified competencies
- Outcome 5 - Incomplete evidence presented - additional training time may be required.
- If you receive an outcome 5, you will be asked to provide additional information within a specific, short-term timeframe. After presentation of the extra evidence, the ARCP panel will update your ARCP outcome to either an outcome 1, 2, 3, 4, 6 or 8 depending on the additional evidence you have provided
- Outcome 6 - Gained all required competencies for the stage of training - will be recommended as having completed the training programme (core or specialty) and if in a run-through training programme or higher training programme, will be recommended for award of CCT or CESR(CP).
- Outcome 8 - Out of programme for clinical experience, research or a career break (OOPE/OOPR/OOPC)
- Not Assessed (N code)- There are circumstances when an ARCP panel is not able to recommend an outcome. For example if a trainee is absent due to statutory leave. In these cases, the ARCP panel will record the reason why no ARCP outcome could be recommended.
Can I appeal my outcome?
Yes, you can appeal any outcome. The process for appealing in detailed here.
I’m worried about my ARCP-who can I speak to?
You can discuss any worries or concerns with your educational supervisor and your college tutor. They will be able to either help you or direct you appropriately to someone who can.
How to document reflection
Reflection is an important part of all doctors' professional development and is especially important when things have not gone well. It can be documented as a personal activity (reflection) in the library on the LLP or as a file uploaded as a personal activity (reflection). It should be assigned to the ARCP on the ESSR under the heading of Personal Reflection. No personal identifiers should be included, and it should focus on lessons learnt.
Helpful guidance includes The Reflective Practitioner guidance and toolkit, jointly developed by the Academy of Medical Royal Colleges, the UK Conference of Postgraduate Medical Deans, the General Medical Council, and the Medical Schools Council.
What forms do I need for my ARCP as an academic trainee?
Please use the LLP and ESSR to prepare for your ARCP in the same way as other trainees. In addition, the Academic Progress Report (attachment at bottom of page) is to support the annual review of any trainee who, since their previous ARCP has been:
-
in an Academic Clinical Fellowship or Clinical Lecturer post; or
-
registered for MD(res), MPhil. or PhD; or
-
undertaking any training, trust grade or fellowship post with ≥25% WTE (usually 12 hours per week) dedicated to research; or
-
out of programme for research (OOPR) or OOPE with ≥25% WTE research
Please upload the completed Academic Progress Report form to your LLP one week before your ARCP date.
I wish to speak to my TPD about my training plans.
Historically the ARCP was a time when changes to training placements or future training plans were discussed with the TPDs, but now that ARCPs are in absentia this does not happen at this time. The TPDs recognise that the opportunity to have a face to face or virtual meeting is very valuable and therefore TPD clinics will be organised usually a few weeks after ARCPs have finished. If you are unable to attend the clinic and your Educational Supervisor or College Tutor cannot help then please contact the TPD who will arrange a virtual face to face appointment on an alternate date if it is required.